Wicked problems - Healthcare
Written by Tom Varghese
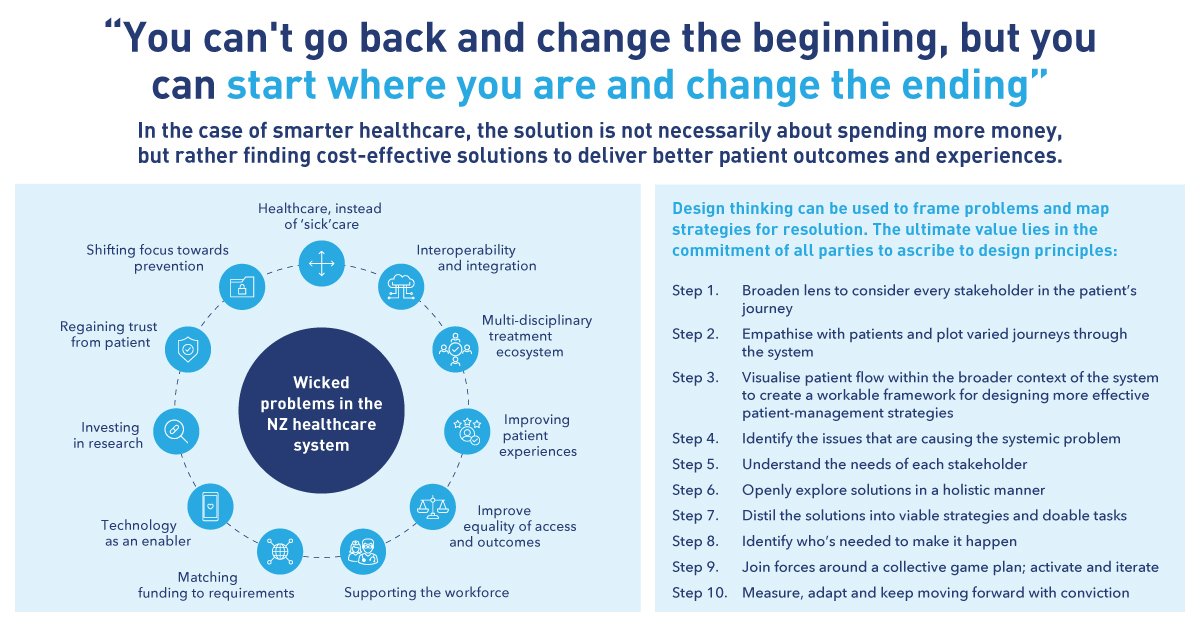
In 1973, Rittel and Webber introduced the term ‘wicked problem’ into social planning vocabulary. Wicked issues are different because traditional processes can’t resolve them. A wicked problem has innumerable causes, is tough to describe, and doesn’t have a right answer. Healthcare is a prime example.
In New Zealand, we have known and tried to address some of the wicked problems in healthcare such as costs, inequities, inconsistencies, timeliness, innovation, resource availability and allocation, and others for many years. The New Zealand health system has undergone more than three decades of major restructuring. Since 2000 a greater emphasis has been placed on primary health care, a strategic health system response to building health equity. A population health approach and social policies directed at closing the health gap have also been features of system restructuring.
Perhaps, focusing on a handful of critical success factors can facilitate reinvention and innovation despite today’s chaotic healthcare environment. The process starts and ends with having the patient’s best interests in mind. This means looking at problems through the patient’s eyes, becoming a partner in their care, and framing products and services that align. Understanding why people do what they do, is the starting point.
The experience journey extends from reducing wait times and claims errors to supporting them with wellness programs to achieve lifestyle changes. It is important to approach any problem in the context of transforming the way people experience health and healthcare.
As organisations seek to innovate and reinvent themselves, they should also be cautious not to rely on a cookie-cutter approach. The success we see in designing new methods for value and access for patients are successful because they have been invented and not merely copied. Sustained innovation requires a leadership mandate and a sustainable revenue cycle for innovation, proprietary innovation processes, and an infrastructure that plays to the strengths and ambitions of the healthcare enterprise. More importantly, unless changes are supported by a culture and mindset shift, they are rarely sustained long term.