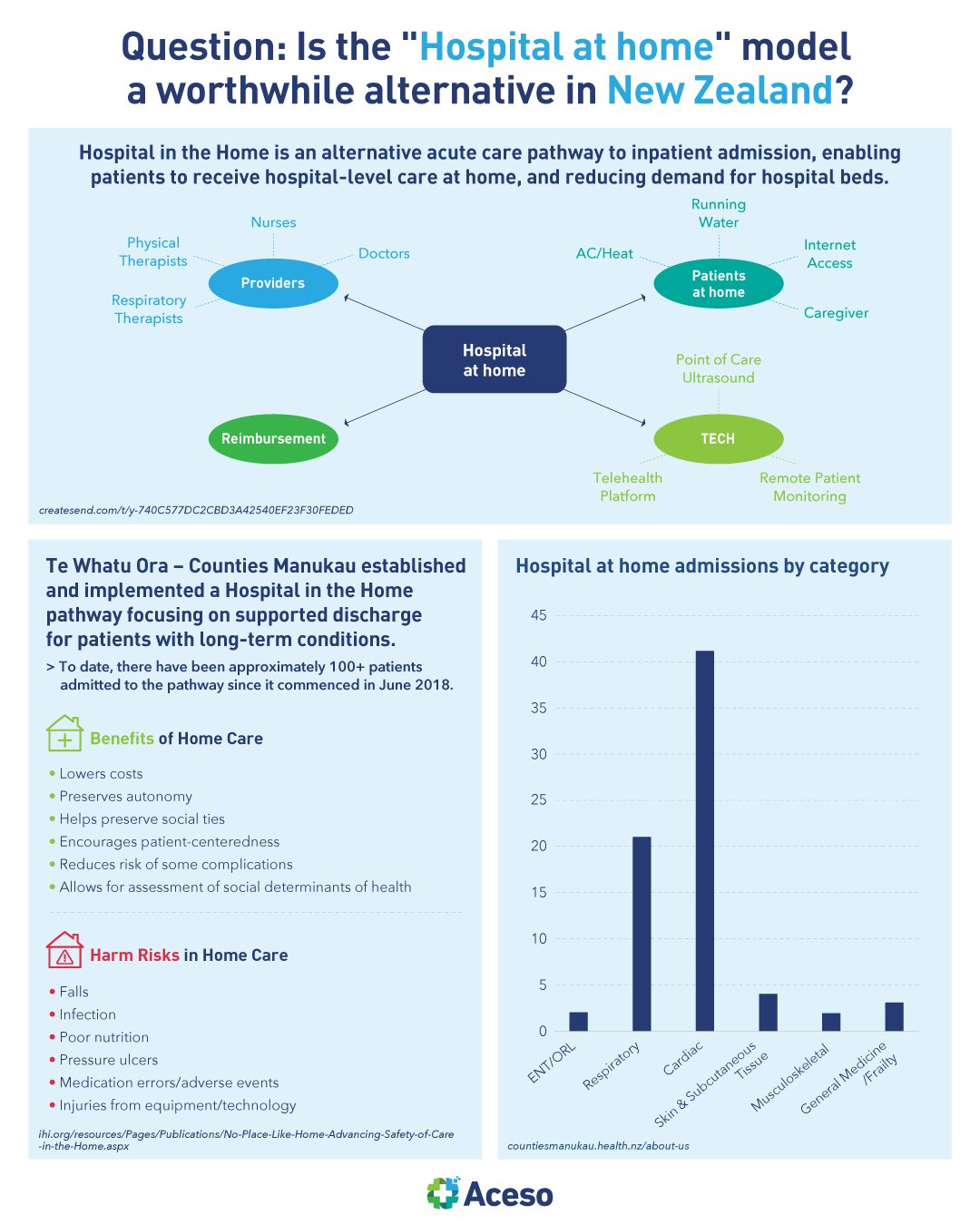
Question: Is the “Hospital at home” model a worthwhile alternative in New Zealand?
Written by Dr. Tom Varghese
Caring for patients in their homes holds many potential benefits, yet the safety of care provided in the home has not received as much attention as patient safety in hospitals and other clinical settings.
Demand for hospital beds has been steadily increasing over recent years and often exceeds the existing capacity. Optimising people’s access to acute care within community health services, and supporting acute hospital flow by avoiding admission and providing early support to patients and their whānau will take the pressure off the system.
Overseas, Johns Hopkins developed its hospital at home program as a means of treating elderly patients who either refused to go the hospital or were at such risk of hospital-acquired infections and other adverse events that GPs kept them at home out of concern for their safety. Early trials of its model found the total cost of at-home care was 32% less than traditional hospital care ($5,081 vs. $7,480), the mean length of stay for patients was shorter by one-third (3.2 days vs. 4.9 days), and the incidence of delirium (among other complications) was dramatically lower (9% vs. 24%).
This approach also introduces some complications. It requires using providers who are comfortable treating patients without face-to-face contact, as well as consistent and continuous communication among team members who operate in a virtual manner. Time constraints are another barrier. Primary care providers who refer patients to the program must screen them carefully and make arrangements to introduce them to the concept of at-home hospital care. For many, it's simply easier to admit patients.
Across one former DHB, the Community Health Teams support patients and their whānau by enhancing their transition to community care, and ensuring patients can manage safely at home, with adequate supports, after they have presented to hospital. Community clinicians also work alongside primary care to increase supports and interventions, as required, so patients can continue to be safely and adequately cared for within their home and community, and to avoid the need for unnecessary hospital presentations. This model of care provides flexibility for patients and enables more care to be delivered outside of the hospital.
The goal is to fully establish a Hospital in the Home model of care that supports the hospital system by providing a greater level of acute care within the community. This will be done through supported discharge and admission avoidance.
In another similar use case, last year, during the pandemic, Auckland DHBs operated a Hospital in the Home programme for Covid-19 patients, keeping whole wards full of people out of hospital. Devices and data were also supplied to patients if needed for them to remain safely at home.
After all, there is no place like home!