How do we accelerate healthcare interoperability standards in New Zealand?
Written by Dr. Tom Varghese
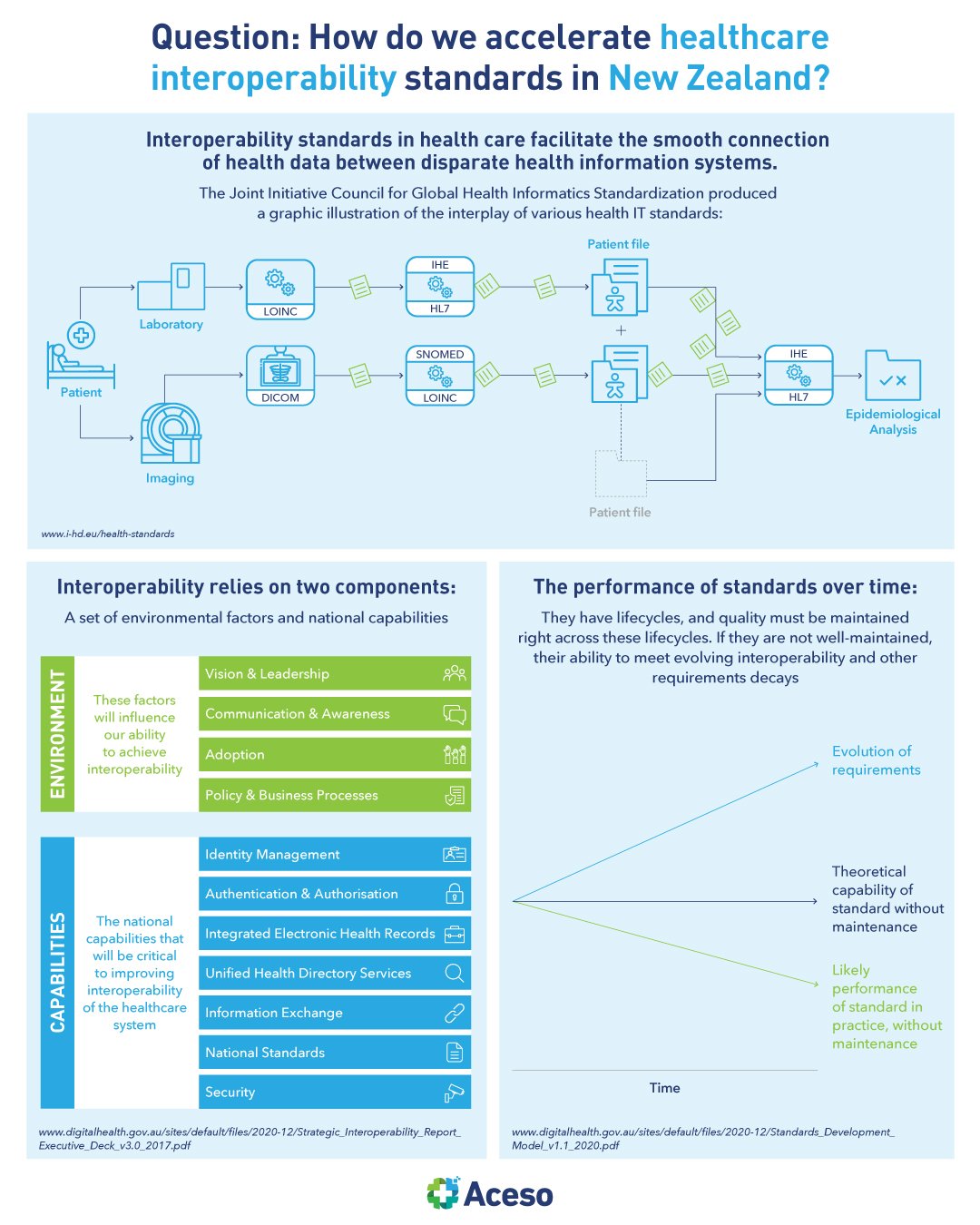
Professionals working in the health care sector record your health data in their digital information systems. Exchanging health information between providers is vital to ensure continuity of care. Equally important, is the exchange of health data with clinical laboratories, pharmacies and disease registries. This is where interoperability standards come in.
Standards pervade virtually every aspect of our lives, whether we realise it or not. They are embedded in virtually every product and service we consume, however they are also often invisible.
Lack of interoperability is widely acknowledged to be a critical barrier for the adoption and deployment of digital health technologies and for the digital transformation of healthcare. Addressing and overcoming this barrier requires awareness and cooperation among all stakeholders. This should start with a shared understanding of the relevant interoperability standards in digital health.
There is not one single digital health interoperability standard. Instead, there is a diversity of standards, specifications and profiles coming from various organisations and initiatives, many of which have organically emerged and grown to meet interoperability needs around specific uses. This has resulted in a fragmented environment leading to uncertainty. While other industries such as mobile communications, aviation services and banking have delivered tangible examples of interoperable data flows while preserving competition, healthcare appears to lag behind.
Why is health information sharing so erratic, when virtually all health data is computerised? Other industries have figured this out. Why not healthcare? The reasons are many and complex. Many healthcare software vendors have made a lucrative business out of creating custom interfaces to connect diverse systems, with billable tweaking every time the provider acquires a new application or upgrades an existing one.
It isn’t that the healthcare industry lacks data standards; quite the opposite. But they are often created by groups with interests in specific types of data. The field of health data interoperability is often perceived as a largely technical endeavour, attracting little clinical interest. In reality, the sharing of patient health data between health and care providers, and organisations, could not be more clinically significant.
A lack of standardised clinical processes and poor quality, incomplete data, without structure and appropriate coding frequently results in an inability to confidently understand what was meant by other health and care providers. At best, this results in significant inefficiency. At worst, providers can make wrong decisions based on an incorrect understanding of diagnoses or medications, causing harm.
In NZ, the Health Information Standards Organisation (HISO) supports and promotes the development and adoption of fit-for-purpose health information standards. HISO works across the sector, and also links with the international standards community through the SNOMED International for SNOMED CT, and through HL7 NZ for HL7 standards.