Are we doing enough to retain our health workforce?
The New Zealand health system is staffed by hardworking, highly trained and committed professionals who deliver excellent care. But over successive decades, we have not grown and supported our workforce to the extent needed. Even though we have seen continuous growth over the past decade, this has left us today with a material gap, and a workforce under strain.
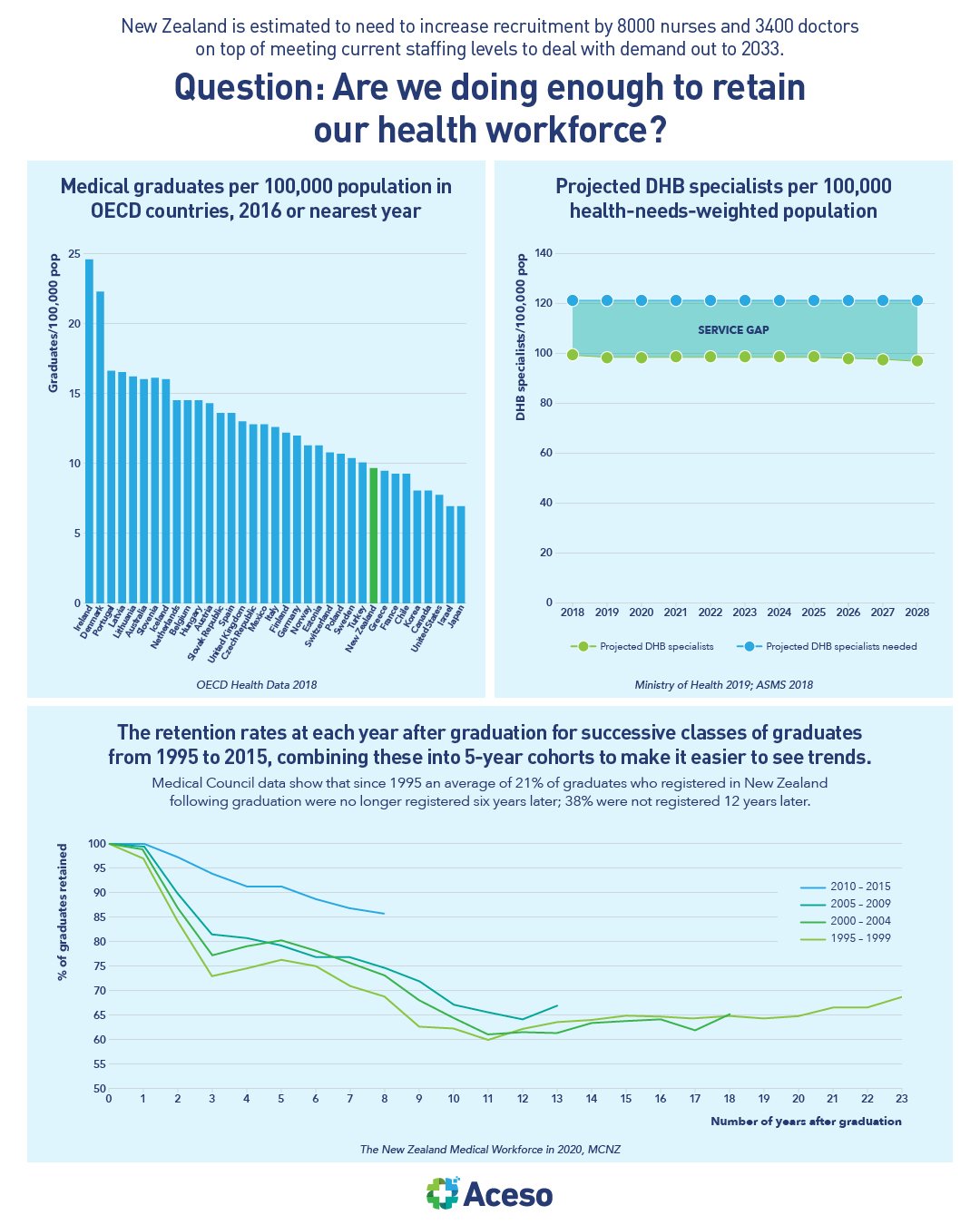
Te Whatu Ora Health NZ estimated Aotearoa was currently short by 4800 nurses, 1700 doctors, 1050 midwives, 220 dental or oral health practitioners, 200 anaesthetic technicians, 170 pharmacists, 120 sonographers, 30 radiation therapists and 30 clinical or cardiac physiologists. However, the agency estimated another 8000 nurses, 3400 doctors and 250 midwives would be needed to make up shortfalls in health demand out to 2033. This data makes some major assumptions including that our models of care, training pathways and retention approaches will not change. Some specialties will be affected more than others. In two case studies using data on workforce and service use data produced by the MoH, the workload per orthopaedic surgeon will need to increase by 6% by 2028 to match current service levels. This does not take account of the already significant unmet need today. Workloads per ophthalmologist will need to increase by 20%, which again is likely to see a worsening of current levels of unmet need.
The gap has been identified as being driven by an inability for the health system to articulate its workforce need, the fragmentation of the former district health boards, which made it hard to realise economies of scale and make best use of available workforce across the motu, global workforce shortages and systemic underinvestment.
That said, over the past 5 years, we have seen a 22.7% increase in the number of nurses employed by Te Whatu Ora, and a 22.8% increase in the number of doctors. We have seen a 35% increase in graduate nursing salaries and a 43% increase in the top step salary for registered nurses since 2017.
Specialist workforce growth rates are hampered by poor retention rates, especially among newly qualified specialists and International Medical Graduates (IMG) specialists. There is potential to make significant inroads into addressing workforce shortages by designing and implementing effective retention measures, taking into account the specific needs of different sections of the workforce.
It takes time to train new people, to improve retention, and to recruit from overseas. There is no single mechanism which will ensure we have the health workforce we need, so this plan anticipates using all of these levers.